Digital system to help check hospital billing discrepancies
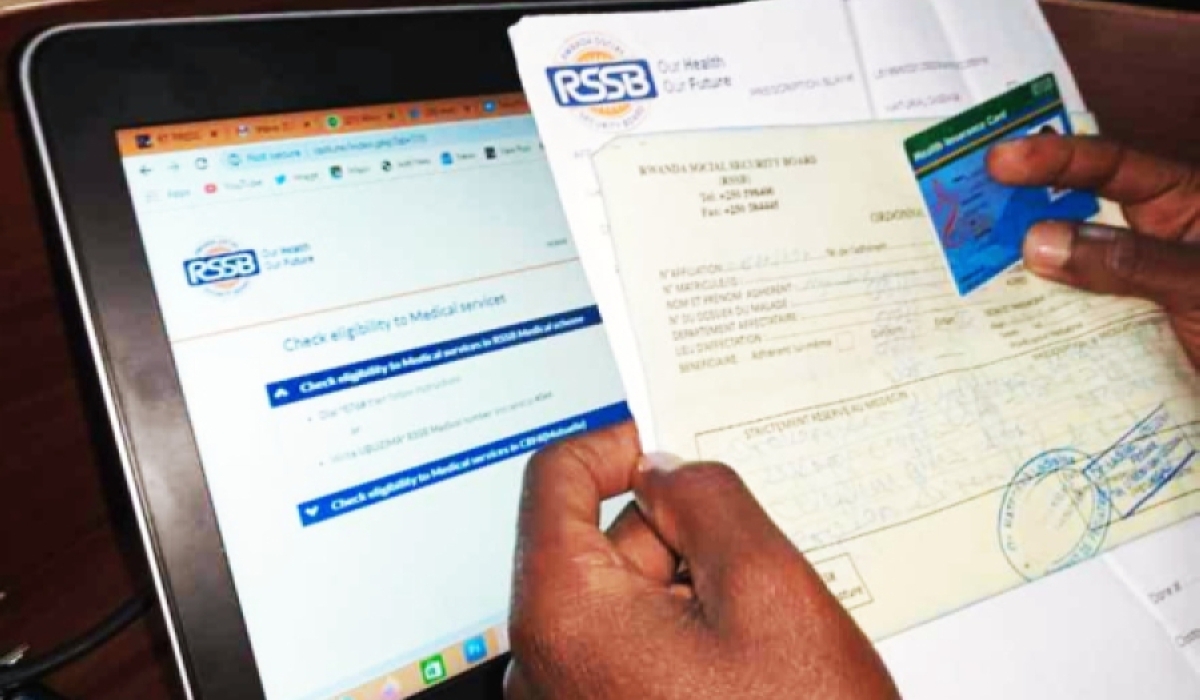
RSSB staff checks the authenticity of documents at the hospital. RSSB is taking proactive measures to address the escalating number of rejected hospital claims by medical insurers and tackle issues related to overbilling.
The Rwanda Social Security Board (RSSB) is proactively addressing the surging number of declined medical claims and tackling issues related to excessive billing by medical insurers through the implementation of a novel digital system for scrutinizing invoices from healthcare providers.
The recent 2022 report from the Auditor General (AG) has highlighted the persistent problem of rejected medical claims by medical insurers, resulting in the loss of billions of Rwandan Francs. The report attributes the rejection of billed amounts to incomplete documentation supporting the claims, usage of expired insurance cards and transfers, billing errors, inclusion of medical services not covered by insurance providers, and discrepancies in interpreting medical invoices or tariff disagreements among insurance staff.
To alleviate the issue, the report suggests that healthcare facilities should ensure due diligence in billing medical insurers and engage the Ministry of Health (MINISANTE) to resolve tariff disagreements. Regis Rugemanshuro, Director General of RSSB, attributes the rejections to overbilling by healthcare facilities or charging for items not covered by insurance. Overbilled items are identified, removed, and subject to a verification process, which is conducted by medical facilities and insurers.
To expedite this process and curb overbilling, RSSB is digitizing the verification process. This initiative aims not only to reduce instances of overbilling but also to accelerate the verification and payment process, shortening the current contractual period of 60 days to just 15 days. Rugemanshuro announced that RSSB has already onboarded over 1,026 health facilities and plans to include all partner healthcare facilities and pharmacies by the end of 2023.
The AG's report also notes that hospitals are experiencing delays of up to 317 days to bill private insurance companies for invoices totaling Rwf8.38 billion in 20 public hospitals. This delay has a negative impact on hospitals' liquidity, necessitating district hospitals to prioritize timely invoicing to maintain smooth cash flows and operational efficiency.



